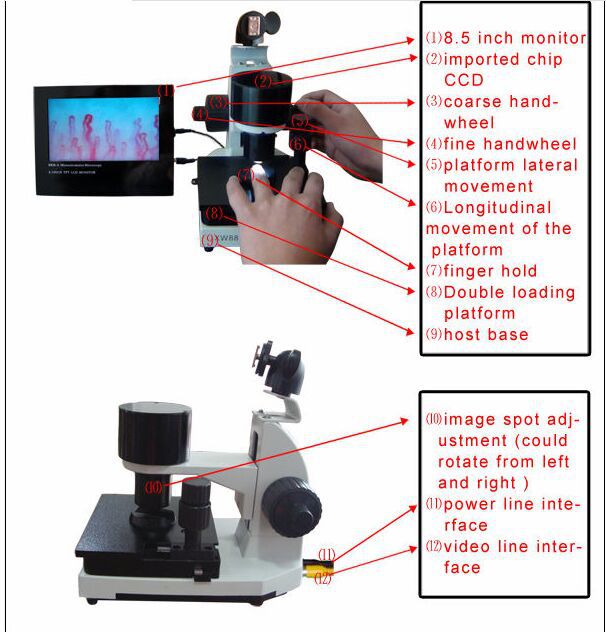
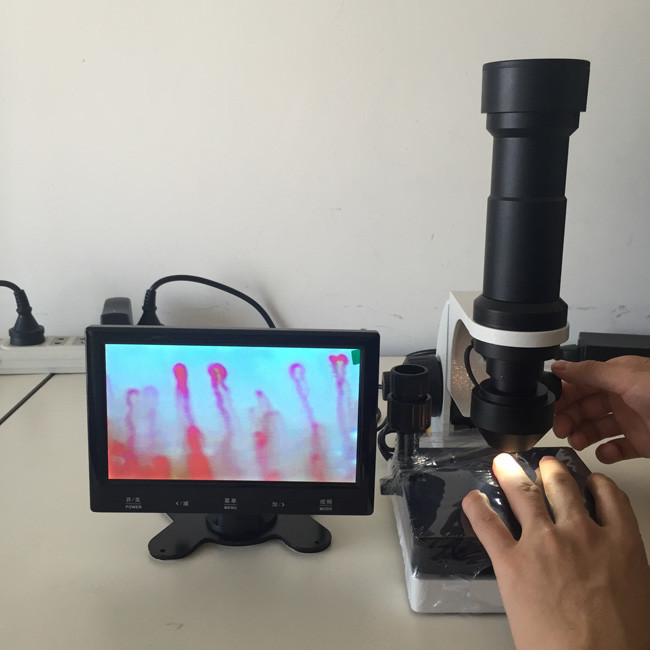
nailfold capillary microscopy
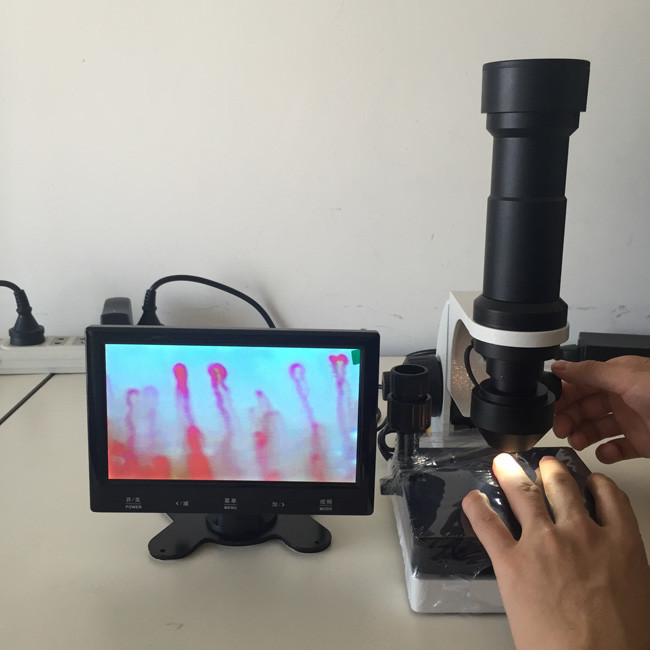
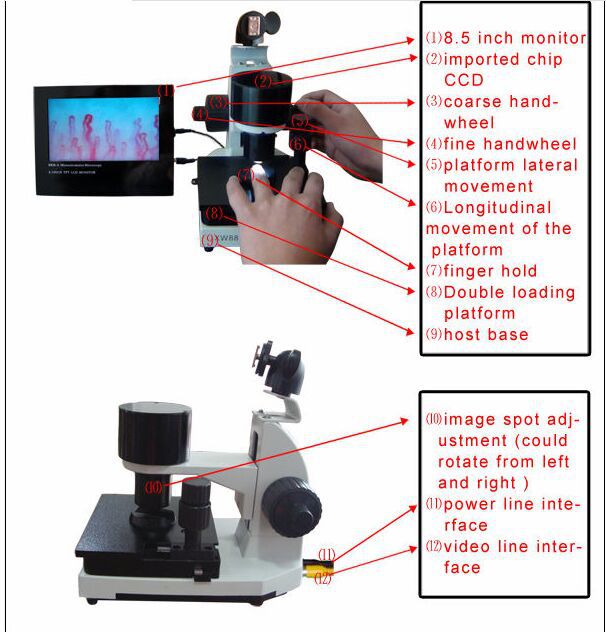
What is nailfold capillary microscopy?

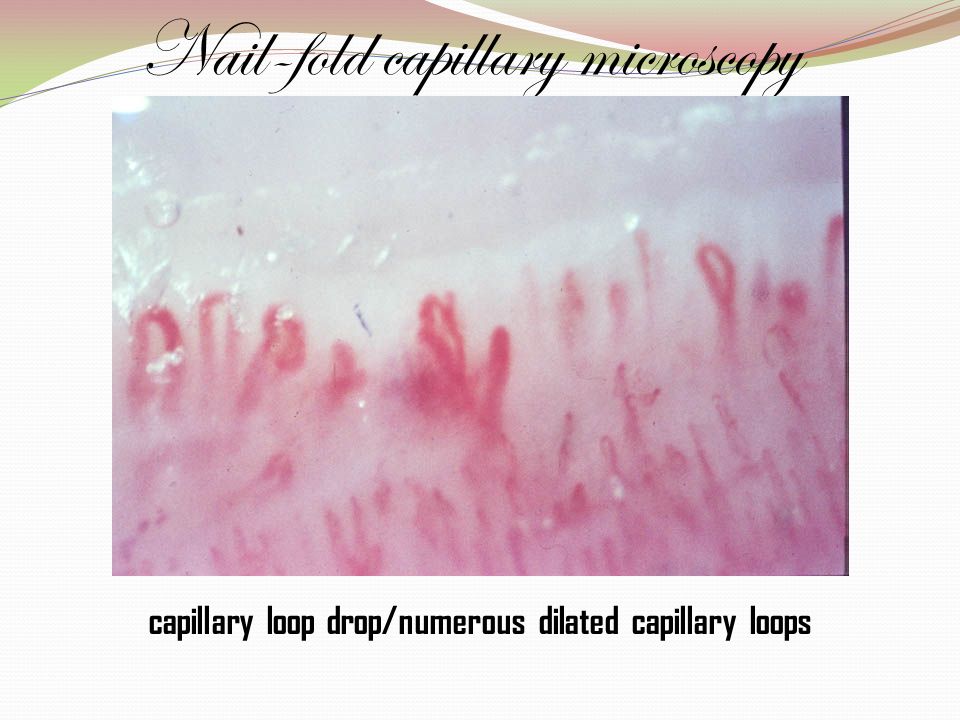
Raynaud’s phenomenon (RP) represents the most frequent clinical aspect of cardio/microvascular involvement and is a key feature of several autoimmune rheumatic diseases. Moreover, RP is associated in a statistically significant manner with many coronary diseases. In normal conditions or in primary RP (excluding during the cold-exposure test), the normal nailfold capillaroscopic pattern shows a regular disposition of the capillary loops along with the nailbed. On the contrary, in subjects suffering from secondary RP, one or more alterations of the capillaroscopic findings should alert the physician of the possibility of a connective tissue disease not yet detected. Nailfold capillaroscopy (NV) represents the best method to analyse microvascular abnormalities in autoimmune rheumatic diseases. Architectural disorganization, giant capillaries, haemorrhages, loss of capillaries, angiogenesis and avascular areas characterize >95% of patients with overt scleroderma (SSc). The term ‘SSc pattern’ includes, all together, these sequential capillaroscopic changes typical to the microvascular involvement in SSc. The capillaroscopic aspects observed in dermatomyositis and in the undifferentiated connective tissue disease are generally reported as ‘SSc-like pattern’. Effectively, and early in the disease, the peripheral microangiopathy may be well recognized and studied by nailfold capillaroscopy, or better with nailfold video capillaroscopy (NVC). The early differential diagnosis between primary and secondary RP is the best advantage NVC may offer. In addition, interesting capillaroscopic changes have been observed in systemic lupus erythematosus, anti-phospholipid syndrome and Sjogren’s syndrome. Further epidemiological and clinical studies are needed to better standardize the NCV patterns. In future, the evaluation of nailfold capillaroscopy in autoimmune rheumatic diseases might represent a tool for the prediction of microvascular heart involvement by considering the systemic microvascular derangement at the capillary nailfold.

nailfold capillary microscopy Introduction
The story of capillaroscopy ‘started’ from the observations of an Italian physician, Giovanni Rasori (1766–1837), who described the close relationship between conjunctival inflammation and the presence of an ‘inextricable knot of capillary loops’ by a magnifying glass .During the beginning of the 20th century, Brown and O’Leary used the capillaroscopic analysis to show in detail the abnormalities that characterize the involvement of microvasculature during Raynaud’s phenomenon (RP) in systemic sclerosis (Ssc). In 1973, Maricq et al. published the first article in Arthritis and Rheumatism, describing the specific capillaroscopic patterns in Ssc as well as the modification of the capillary blood flow during cold exposure, both in primary and secondary RP . Nailfold videocapillaroscopy (NVC) represents the best method to analyse micro/cardiovascular abnormalities in rheumatic diseases. In normal conditions, the microvascular pattern is characterized by a regular array of microvessels with large intra/interindividual variability. However, absolute absence of capillary loss and giant capillaries is expected in normal pattern.Recently, three defined major NVC patterns have been considered useful in assessing the appearance and progression of the sclerodermic microangiopathy (‘early’, ‘active’ and ‘late’ patterns)

nailfold capillary microscopy The ‘scleroderma pattern’
The microvascular damage in SSc is mainly characterized by increasing structural alterations of the capillaries with progressive decrease in their density. Blood flow is also altered, with an average slowing of flow and increased periods of stasis.
Early in the disease, the peripheral microangiopathy may be well recognized and studied by nailfold capillaroscopy or better with the videocapillaroscopy, a non-invasive and safe technique, which is well reported to have both diagnostic and prognostic values in the presence of RP .
Previous studies have partially graded the morphological aspects of the vascular damage in patients with SSc, as assessed by nailfold capillaroscopy, and two major patterns within the term ‘scleroderma pattern’ (SSc pattern) have been recognized from the beginning: namely the ‘active’ and the ‘slow’ patterns.
Further morphological studies have been published more recently.
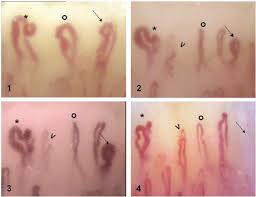
In a recent study, microvascular alterations as detected by NVC in patients with SSc have been re-classified in three different patterns.
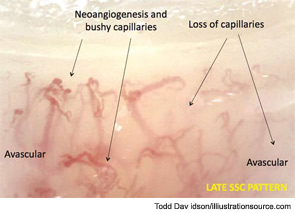
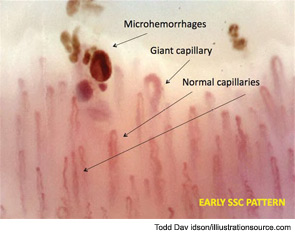
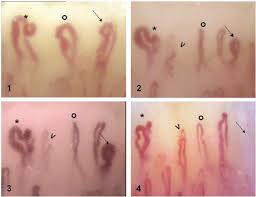
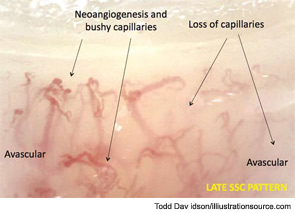
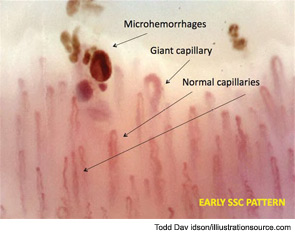
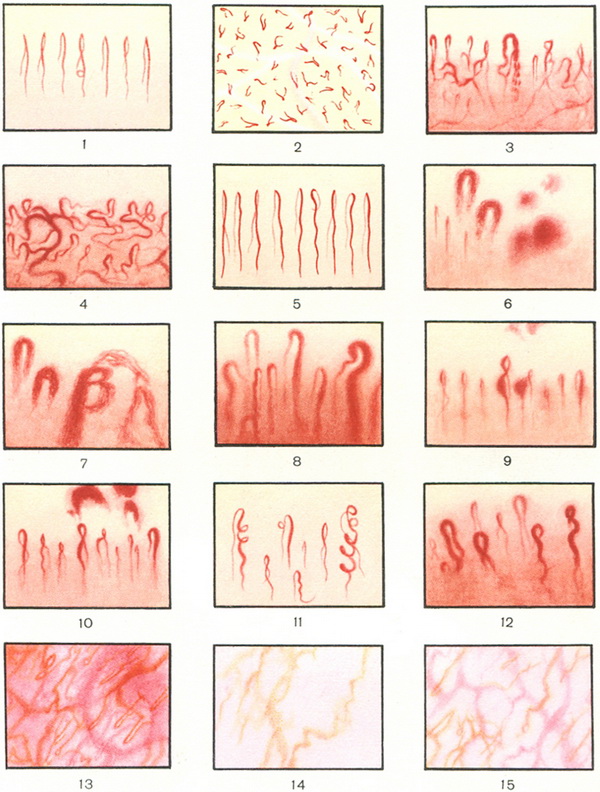
The patterns identified within the ‘SSc pattern’ include: (i) ‘Early’ NVC pattern: few enlarged/giant capillaries, few capillary haemorrhages, relatively well-preserved capillary distribution, no evident loss of capillaries (Fig. 1); (ii) ‘Active’ NVC pattern: frequent giant capillaries, frequent capillary haemorrhages, moderate loss of capillaries, mild disorganization of the capillary architecture, absent or mild ramified capillaries; and (iii) ‘Late’ NVC pattern: irregular enlargement of the capillaries, few or absent giant capillaries and haemorrhages, severe loss of capillaries with extensive avascular areas, disorganization of the normal capillary array, ramified/bushy capillaries
This study confirmed previous observations, indicating enlarged and giant capillaries together with haemorrhages as the earliest NVC finding in SSc. In the late stage of the disease, these abnormalities become rare.
Early stage is also characterized by microvessels with normal diameter coexisting with few enlarged capillaries that must be carefully investigated on all the fingers by considering the limited number of these nailfold changes during early phases of the disease.
Conversely, these changes are strongly increased in SSc patients with an ‘active’ pattern. Loss of capillaries, together with vascular architectural disorganization and ramified capillaries, were found to be rare in the early stages of SSc, whereas they seem to increase with the progression of the fibrotic phase of the disease (‘active’ and ‘late’ patterns).
A significant and gradual increase of these latter vascular abnormalities is observed during the SSc progression, and the three NVC patterns have been found to correlate with both RP and SSc durations, reflecting at least the possible evolution of the disease process .
While in healthy control subjects and in patients with primary RP the morphological features of the nailfold microvascular bed may remain unchanged for a long time, patients with RP associated with SSc-spectrum disorders may, on the contrary, show a higher degree of morphological variability, even after a few days.
The NVC patterns have been correlated with different clinical aspects and manifestations of SSc, as well as to the effects of treatment contributing to the overall study of the disease.

nailfold capillary microscopy Capillaroscopic patterns and rheumatic diseases
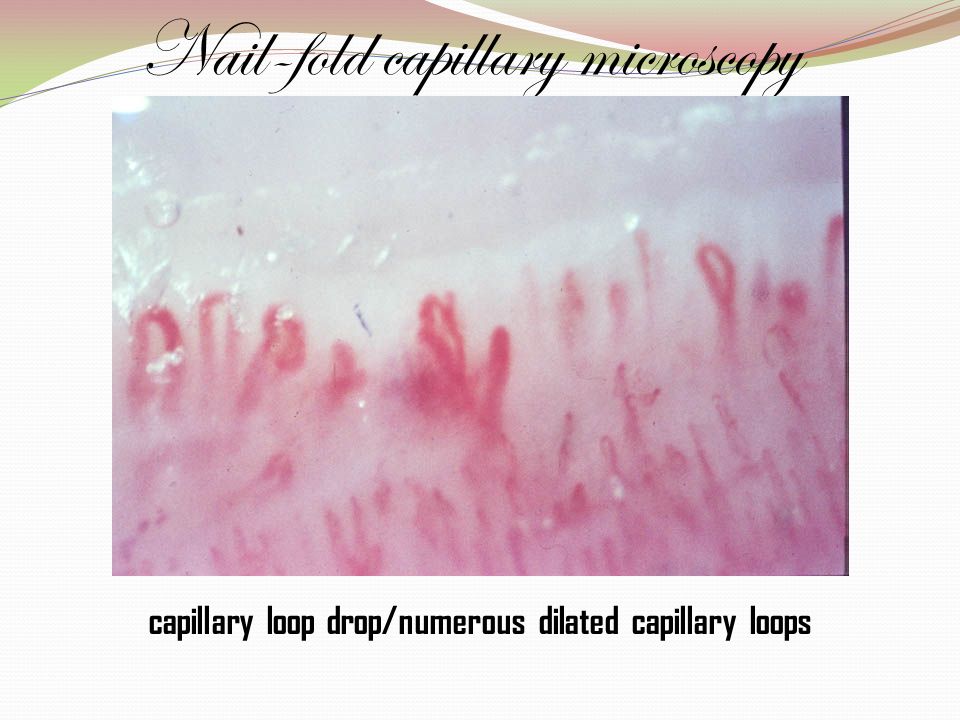
The presence of megacapillaries and a decreased capillary density are the hallmarks of the SSc capillary pattern, which can be detected by nailfold capillaromicroscopy.
However, in a recent large study, 186 patients with RP, 65 with undifferentiated connective tissue disease (UCTD), 47 with systemic lupus erythematosus (SLE), 26 with dermato/polymyositis, 14 with rheumatoid arthritis, 7 with primary Sjogren’s syndrome (SS) and 102 patients with SSc were investigated.
Of the 16 patients with diffuse cutaneous SSc and the 86 with limited cutaneous SSc, 14 (87.5%) and 53 (61.6%), respectively, showed the SSc capillary pattern.
Nine of the 65 (13.8%) cases with UCTD and 24 of the 186 (12.9%) cases with RP also exhibited the same pattern.
Four of the 47 (8.5%) patients with SLE and seven of the 26 (26.9%) with dermato/polymyositis, and no patients with rheumatoid arthritis or SS exhibited the SSc capillary pattern.
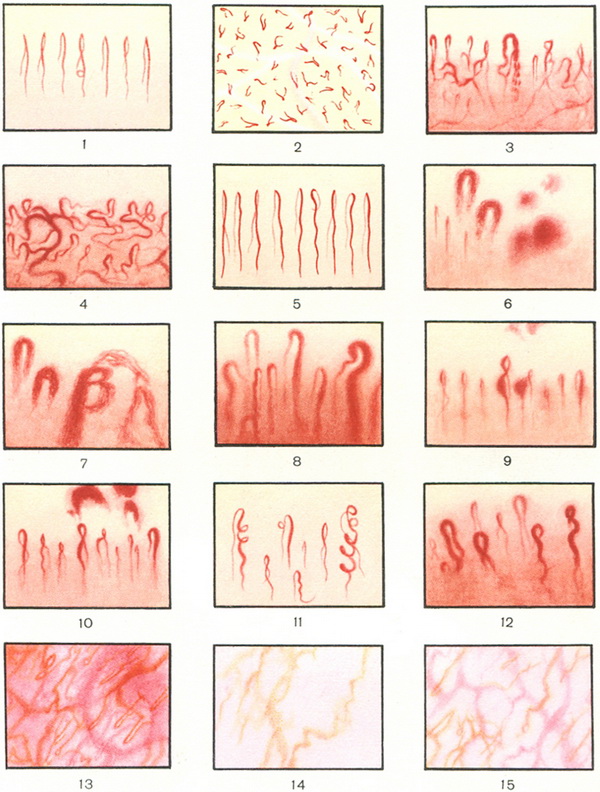
The conclusion is that the ‘SSc pattern’ is often present in SSc and dermato/polymyositis. Furthermore, patients with RP and UCTD may also exhibit this pattern occasionally (Fig. 2B). Therefore, capillaromicroscopy seems to be a useful tool for the early selection of those patients who are potential candidates for developing SSc spectrum disorders.
Dermatomyositis
A defined pattern has been reported in patients affected by dermatomyositis (DM). This pattern, often associated with aspects of the SSc pattern, includes the presence of two or more of the following findings in at least two nail folds: enlargement of capillary loops, loss of capillaries, disorganization of the normal distribution of capillaries, ‘budding’ (‘bushy’) capillaries, twisted enlarged capillaries and capillary haemorrhages (extravasates) (Fig. 2C).
Systemic lupus erythematosus
Characteristic SLE pattern includes morphological alterations of capillary loops, venular visibility and sludging of blood with variability of capillary loop length. A recent study evaluated the association between nailfold capillary abnormalities frequently observed in SLE patients and the presence of RP, anti-U1-ribonucleoproteins (RNP) and anti-cardiolipin (aCL) antibodies.
One hundred SLE patients were studied. The widefield nailfold capillaroscopy was considered abnormal according to five criteria. Intercapillary distance, capillary width and capillary length were registered by videomorphometry in two fingers in all the 100 patients and in four fingers in 40 of them. Both the presence of altered capillaroscopy and that of the SSc pattern, characterized by the presence of avascular areas and enlarged or giant loops, were associated with the isolated presence of RP (P < 0.001) or anti-U1-RNP antibodies (P < 0.01), as well as with the simultaneous presence of RP and anti-U1-RNP antibodies (P < 0.001). There was a negative association between the presence of aCL antibodies and SSc pattern (P < 0.05). Higher figures for the videomorphometric parameters capillary width, intercapillary distance and capillary length were observed in patients with RP. Patients presenting both RP and anti-U1-RNP antibodies showed higher figures for intercapillary distance and capillary width. This study demonstrated significant association between nailfold capillaroscopic abnormalities and either RP or anti-U1-RNP antibodies in SLE patients. The association of RP, anti-U1-RNP antibodies and ‘SSc like’ findings on nailfold capillaroscopy (SSc pattern) in patients with SLE may suggest a new SLE subset with subclinical features of SSc.
A previous study evaluated the relationship between aCL (found in about 40–50% of patients suffering from SLE) and skin microcirculatory changes or vascular symptoms in 51 consecutive SLE patients.
Twenty-two patients (43.1%) had positive aCL [immunoglobins G (IgG) 22 (5–60) G phospholipids (GPL); immunoglobins M (IgM) 5 (3–16.5) M phospholipids (MPL); median titre and range, respectively] and 12 (54.5%) of them had abnormal capillaroscopic findings. In contrast, among the 29 patients without aCL, only six (20.7%) had an abnormal capillaroscopy (P = 0.027). There was no correlation between either aCL or capillaroscopy and RP. These results showed a relationship between aCL and nailfold capillary changes in patients with SLE, suggesting a direct damage of the vascular endothelium by aCL.
nailfold capillary microscopy Anti-phospholipid syndrome
As a matter of fact, interesting microvascular alterations have been observed in patients affected by anti-phospholipid syndrome (APS). One study reported symmetrical microhaemorrhages at nailfold analysis, which were found particularly significant in patients showing the presence of both serum IgG and IgM ACL (Fig. 2D). Marked microcirculatory damage was found in relation with the occurrence of thrombotic manifestations in the APS patients in other studies, confirming the pattern.
A more recent study confirmed that nailfold capillary morphology is altered in patients with APS, but these changes could not be correlated to the impairment of functional parameters.
nailfold capillary microscopy Sjogren’s syndrome
Capillaroscopic changes have been observed also in primary SS. Forty patients with SS (14 without RP, 16 with RP, 10 with ACA), 20 patients with SSc (10 with limited and 10 with diffuse disease) (disease control group) and 40 healthy controls (control group) were evaluated by nailfold capillaroscopy. Capillaroscopic abnormalities in SS ranged from non-specific findings (crossed capillaries) to more specific findings (confluent haemorrhages and pericapillary haemorrhages) or SSc-type findings. SS patients with RP presented capillary abnormalities in higher frequency than patients without RP. The majority of SS patients with ACA (80%) presented SSc-type findings. Nailfold capillaroscopy can be used as a simple non-invasive method to evaluate the microvascular abnormalities in SS patients, especially in those with RP and with ACA.
Conclusions
Since in a recent study, duplex determination of the carotid elasticity or stiffness was found significantly impaired in secondary RP associated with SSc when compared with primary RP, the early capillaroscopic differential diagnosis between the two forms might improve the cardiac prognosis.
In fact, the recognition of the capillaroscopic patterns characterizing the secondary RP might be prognostic even for the early detection of the risk of visceral RP (i.e. coronary heart disease).
In conclusion, the regular evaluation of nailfold capillaroscopy in autoimmune rheumatic diseases will represent soon a tool for the analysis even of the microvascular heart involvement by considering the systemic involvement of the microvessels in these diseases.

Related Items