nail fold telangiectasia : why and how to treatment
nail fold telangiectasia

What is Telangiectasia?
Telangiectasias are dilated blood vessels located near the surface of the skin or mucous membranes. They often appear as fine pink or red lines, which temporarily whiten under pressure. Matted telangiectasias are clusters of these small dilated blood vessels that form a pink or red patch on the skin. Although otherwise healthy individuals may develop this condition, telangiectasias are a cardinal feature of systemic and limited scleroderma, as well as dermatomyositis.Acquired Causes of Telangiectasias,Telangiectasias in Scleroderma, Dermatomyositis, and LupusVisiting Your Doctor Prevention and Treatment.
Why nail fold telangiectasia?
Acquired Causes of Telangiectasias
There are many causes of telangiectasias. Perhaps most commonly, telangiectasias are found in areas of chronic sun damage in fair-skinned individuals. They can also be seen on the sides of the nose in healthy adults.
Conditions associated with telangiectasias include:
Rosacea
Pregnancy
Liver Disease
Chronic systemic or topical corticosteroid use

Connective tissue diseases associated with telangiectasias include:
Scleroderma
Dermatomyositis
Telangiectasias in Scleroderma, Dermatomyositis, and Lupus
Connective tissue diseases often cause telangiectasias to develop on the face and fingernail folds (where the skin meets the nail).
Scleroderma
Patients with scleroderma may develop telangiectasias on the face, mucous membranes, and hands. The condition occurs with both types of scleroderma:
Limited scleroderma, (CREST syndrome – Calcinosis, Raynaud’s, Esophageal Dysmotility, Sclerosis, and Telangiectasia) that affects primarily the skin of the face, hands and feet (with possible involvement of other organs).
Diffuse scleroderma, which has a more rapid onset and affects internal organs as well as the skin.
Telangiectasias become more numerous over time in both types of the disease, however, they are thought to occur more frequently in patients with limited scleroderma.
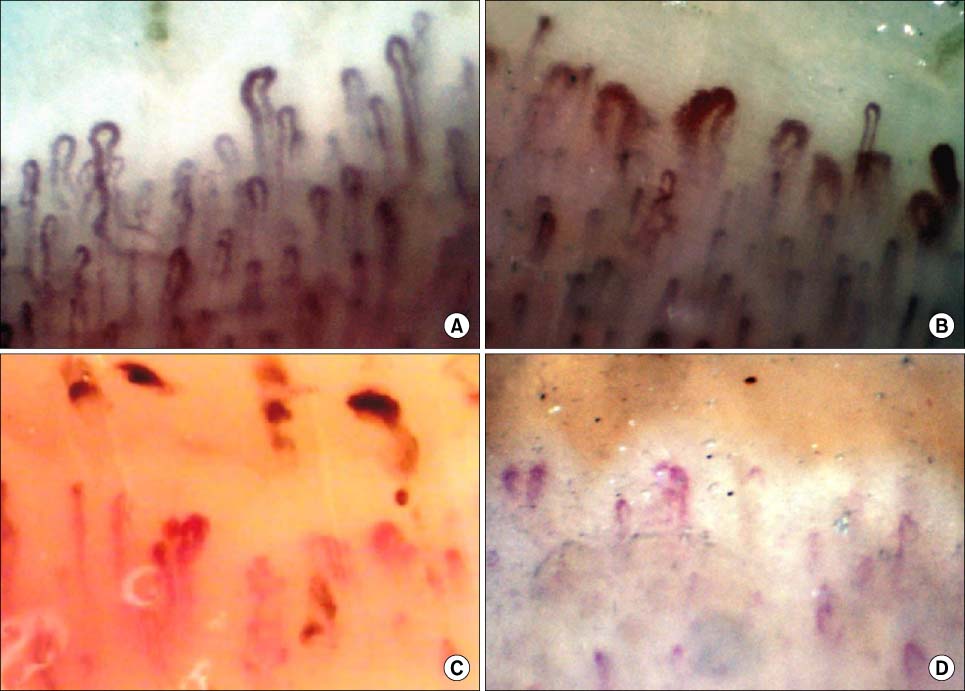
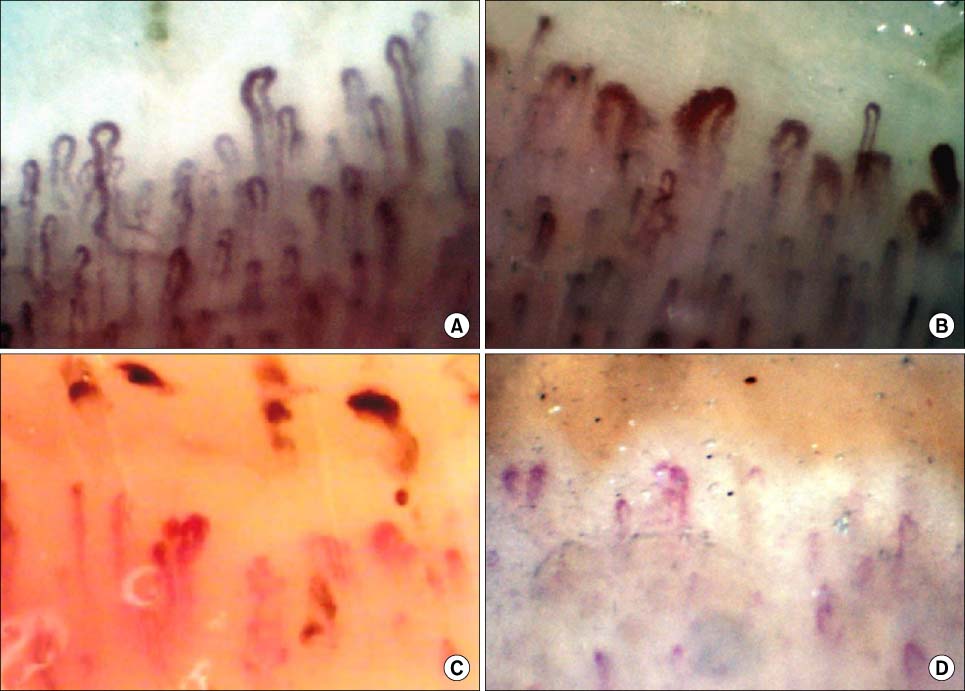
Although the precise factors involved in the development of telangiectasias are unknown, some experts believe that they are a manifestation of the body’s attempt to increase blood flow to organ tissue with poor circulation. Thus, in scleroderma, telangiectasias may be a marker of ongoing vascular injury and failed repair.
Researchers have also identified the following facts and findings about telangiectasias in individuals with scleroderma:
The total number of telangiectasias has been shown to correlate with disease duration; whereas the longer you have had the disease, the more telangiectasias can develop.
The number of talengiectasias also correlates to the risk of developing pulmonary artery hypertension.
Telangiectasias are associated with the presence of the centromere antibody, (an antibody to a portion of the chromosome that is active in cell division).
One study found that body image dissatisfaction was higher in scleroderma patients with numerous telangiectasias.
Dermatomyositis
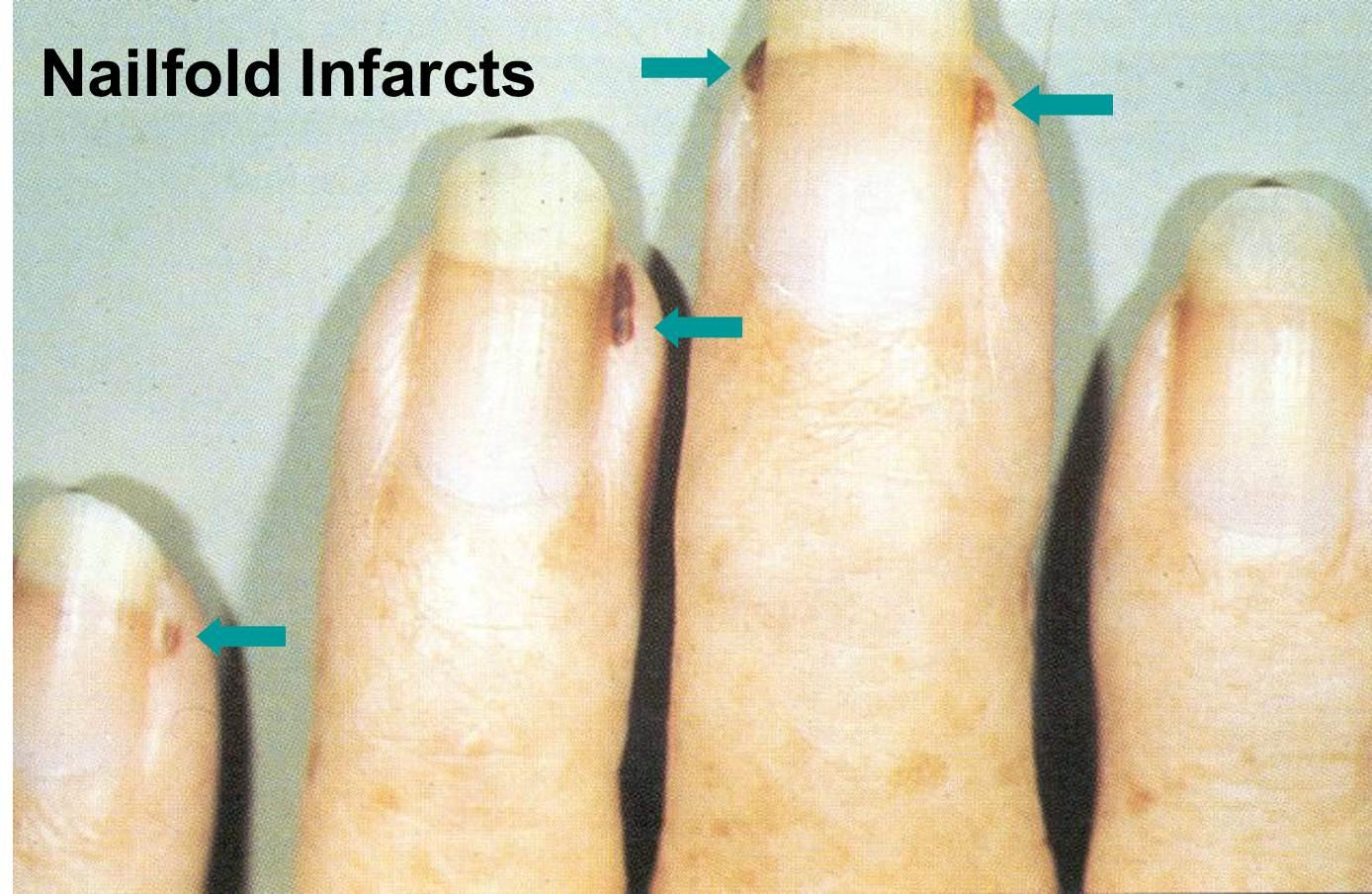
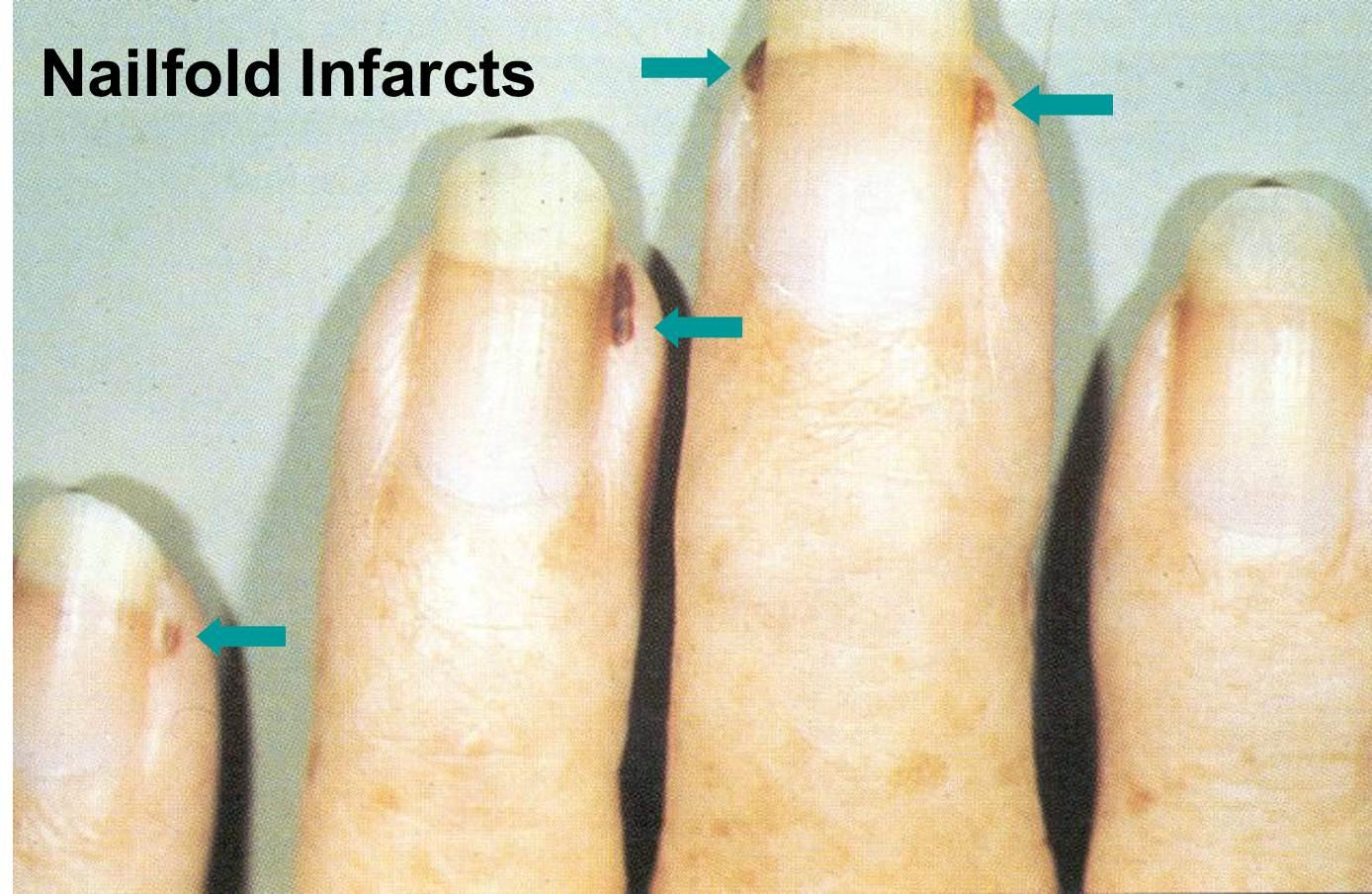
In individuals with dermatomyositis, telangiectasias are typically found in sun-exposed areas, such as the V-shaped area of the neck and chest or in a “shawl” distribution over the shoulders, arms, and upper back. They can be associated with brown discoloration and thinning of the skin, a clinical finding called poikiloderma. This tends to occur in patients with long standing dermatomyositis. Telangiectasias that appear as dilated loops of capillaries with avascular areas (lacking blood vessels) on the fingernail folds are highly characteristic of both scleroderma and dermatomyositis. These findings can help physicians make an early diagnosis of these conditions.
Lupus
Telangiectasias of the nailfolds also occur in individuals with lupus and correlate with systemic disease activity and Raynaud’s phenomenon. Telangiectasias may also be found on the edges of lesions of discoid lupus.
How prevented nail fold telangiectasia ?
Activities that trigger blushing or facial redness can worsen telangiectasias. Although triggers are different for each individual, common culprits include:
ultraviolet radiation
heat
cold
strong wind
alcohol
smoking
hot drinks and food
spicy food
Products that result in irritation of the skin, such as abrasive cleansers, can also worsen telangiectasias.
The following tips are recommended:
Protect skin from the sun with sunscreen, sunglasses, and hats
Use mild cleansers
Minimize exposure to extremes of temperature
Avoid application of topical steroids

How to treatment nail fold telangiectasia?
Although telangiectasias themselves pose no adverse health risk, there are treatments available to improve their appearance.
Cosmetic Camouflage
Cosmetic camouflage is a technique using topical creams or powders to conceal conspicuous skin conditions. Flesh-toned cover-up can immediately hide mild telangiectasias. For more prominent telangiectasias and facial redness, a slightly green-tinted foundation or moisturizer can neutralize the color. These compounds are cost effective and readily available. Look for products with the terms “redness concealer,” “redness relief,” or “redness solutions.” Department stores with large make-up counters will often have a cosmetic therapist (make-up artist) trained to help patients with cosmetic camouflage. He or she will help create a regimen to match individual skin tone and hide telangiectasias.
Laser therapy
This form of therapy uses a specific wavelength of light to selectively heat hemoglobin (the protein responsible for the red color of blood) and seal dilated blood vessels. Superficial facial telangiectasias are amenable to laser treatment. In scleroderma, due to thickened collagen fibers, telangiectasias are more resistant to laser therapy, but can be effectively cleared with multiple treatments. However, this does not prevent new telangiectasias from forming and subsequent treatments may be required to maintain the desired effects. Individuals considering laser therapy for telangiectasias should be aware that insurance plans deem these treatments to be “cosmetic” and do not yet cover this expense.
Electrodessication
Electrodessication entails the insertion of fine needle into the blood vessel. An electrical current is then applied, which seals the vessel. This treatment may be helpful for simple facial telangiectasias; however, it has a higher risk of scarring compared to laser therapy.
Related Items