Why proximal nail fold infection
Why proximal nail fold infection?
Paronychia, commonly known as bacterial nail infection, is inflammation of the region of the finger or toe from which the nail plate originates, which is called the proximal nail fold (PNF). This inflammation may occur in the short term (acute) or may be a long-term problem or one that keeps coming back (chronic).
Acute paronychia develops along a break in the skin and is usually seen at the side of the nail. This type of nail infection is often caused by a bacterial infection but may also be caused by herpes, a type of viral infection.
Chronic paronychia occurs most often in people whose hands are constantly or often exposed to moisture. This disorder often results from contact dermatitis, a type of skin inflammation caused by exposure to chemicals that are irritating to the skin. People with chronic paronychia may have periodic, painful flare-ups. This type of nail infection may be complicated by the addition of a fungal infection, commonly due to a type of yeast called Candida, or bacterial infection, and this may lead to abnormal nail growth.
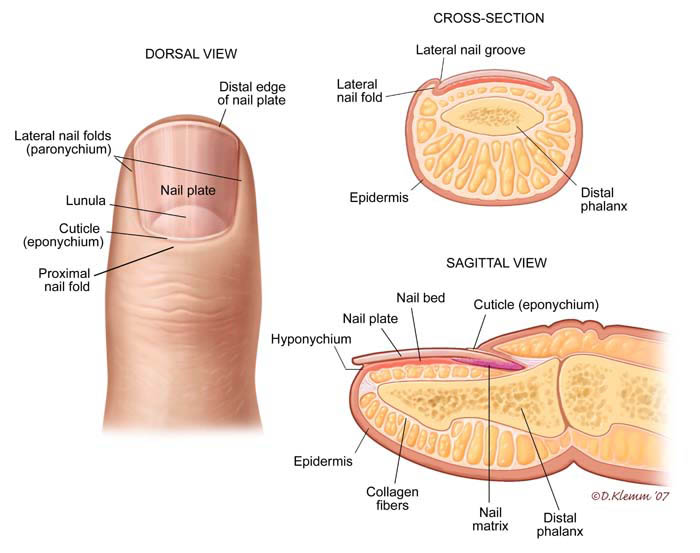
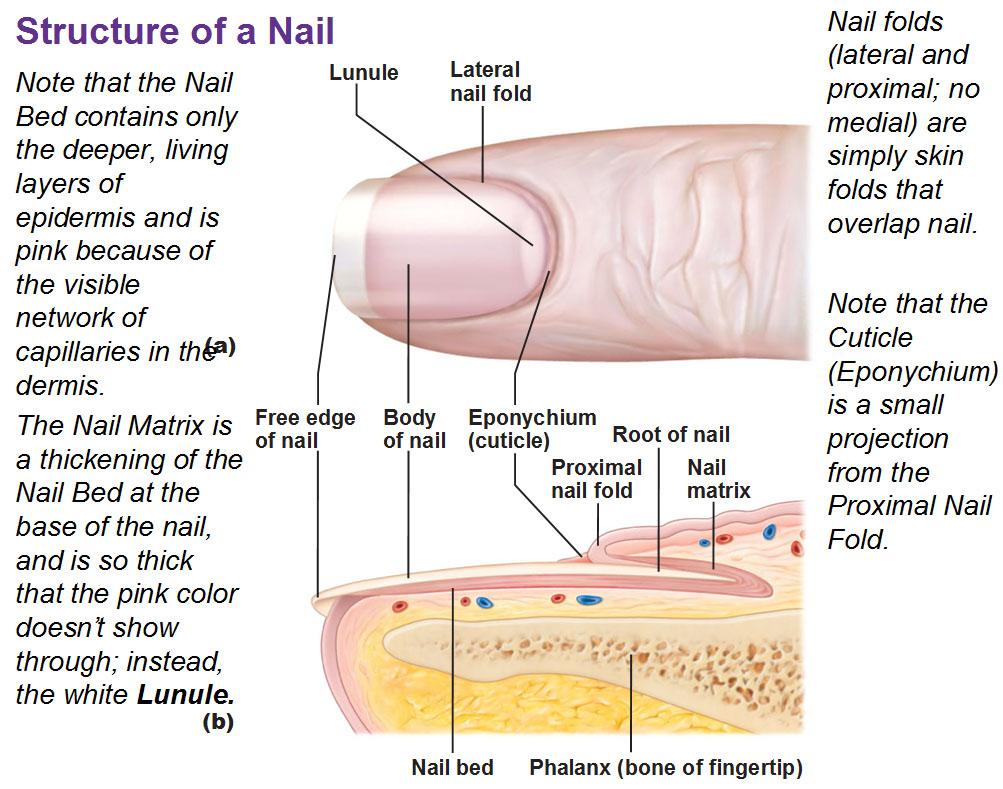
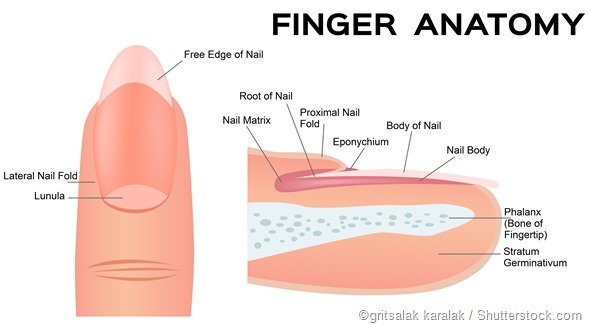
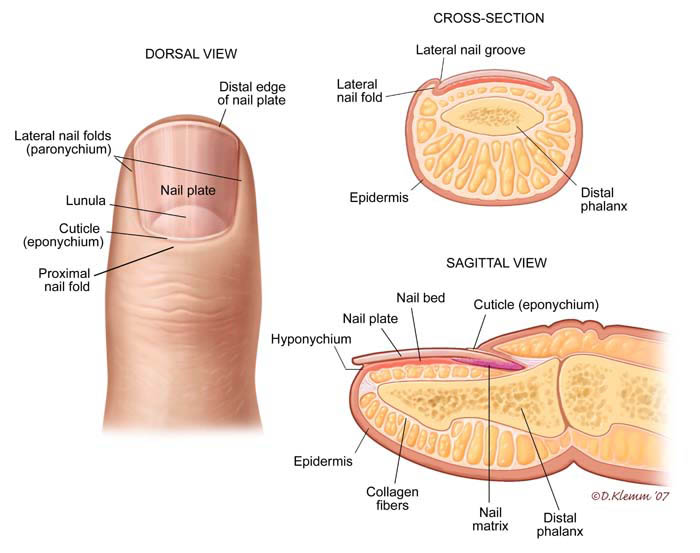
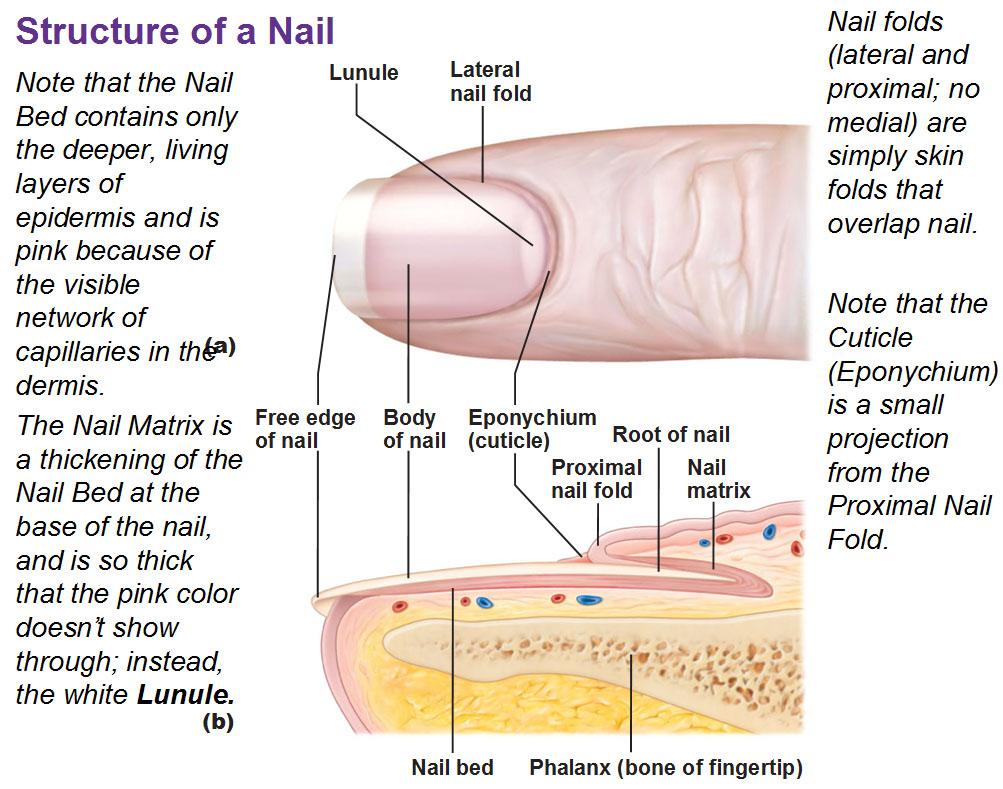
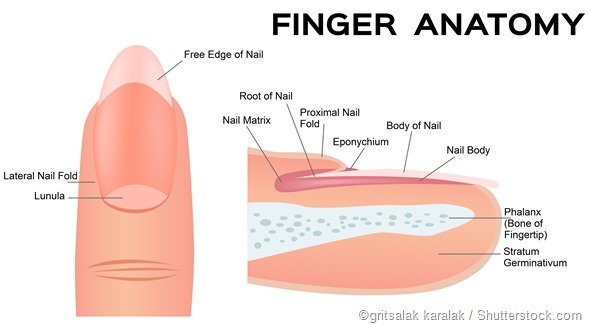
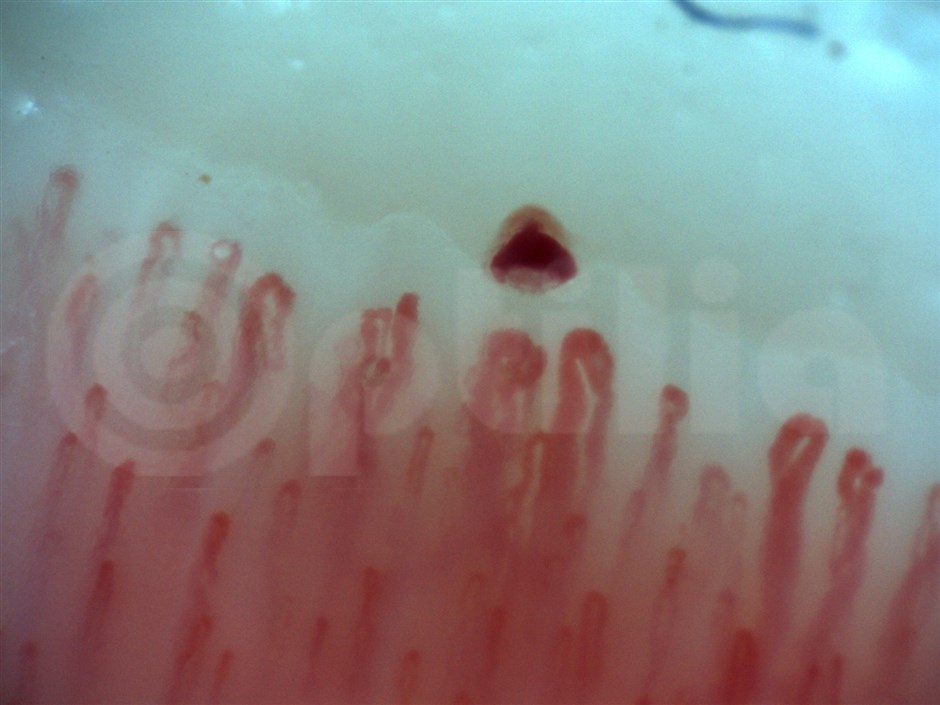
Nail fold infections are best understood by considering the anatomy of the nail. The nail is composed of a keratinized nail plate which lies upon a vascular nail bed. The nail plate keratin is formed by the germinal nail matrix which is at the proximal end of the nail bed.
The nail plate is enclosed at its base by the proximal nail fold, and by the lateral nail folds at both sides. The proximal nail fold has two layers, of which the upper layer is above the nail plate and the lower layer below it.
The upper layer continues as the cuticle, binding the nail plate firmly and impenetrably to the skin just behind it. This cuticular seal prevents moisture and microbes from entering the potential space between the nail plate and the nail fold.
Who’s at risk proximal nail fold infection?
Acute paronychia may occur at any age but is particularly common in children. Viral paronychia occurs more often in adults and may be seen with genital herpes infection or in people who work in the health care industry.
Chronic paronychia is most common in adult women and those who work in places where their hands are kept moist, such as food handlers.
proximal nail fold infection Signs and Symptoms
Bacterial nail infection most often affects the proximal nail fold of the fingers and less commonly affects the toes.
Acute: The proximal nail fold is red, swollen, painful, and may contain pus. Usually one nail is affected.
Chronic: The proximal nail fold is swollen, red, and has no cuticle (the strip of hardened skin at the base and sides of a fingernail or toenail). One or more nails may be affected.
How to do proximal nail fold infection?
Progress of Infection
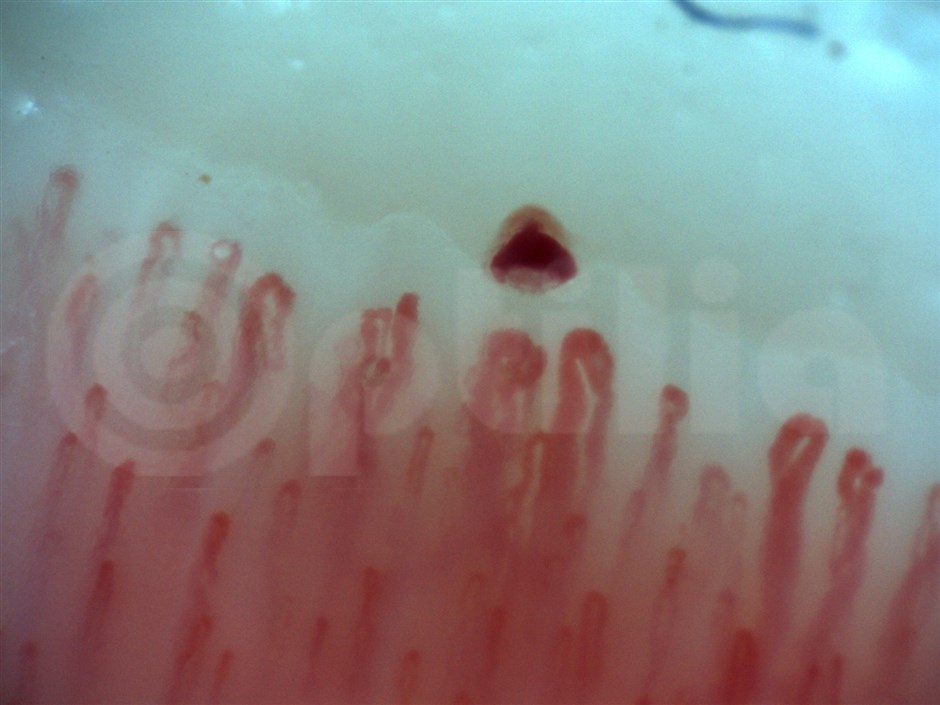
Once the infection has become established, it often produces pus. The pus can form a pocket, called an abscess. In other cases the pus may spread around the nail to produce other abscesses at the side of the nail. It may creep under the nail plate to form more pus between the nail bed and the nail plate, separating the two altogether or in part. In other patients, secondary fungal infection sets in because of the inflammatory conditions.
As the nail fold infection becomes more chronic, it gives rise to altered growth of the nail plate. This results in thickening or discoloration, or the formation of ridges and depressions on the nail. Other nails may also become infected by the spread of the organism to other fingers.
Causes of Nail Fold Infection
Nail fold infection, also called paronychia, is a common condition that occurs when the skin fold at the proximal end of the nail is invaded by bacteria, such as Staphylococcus aureus. Risk factors for such an infection include:
- Constant exposure to moisture
- Cutting back the cuticles too much
- Biting the nails
- The presence of any inflammatory or allergic skin condition near the nails
Such processes either cause trauma to the skin, or lower the effectiveness of the normal skin barrier to microbes.
Individuals who are occupationally forced to spend much time with their hands in water, detergents or other chemicals are at a higher risk of developing nail fold infection. This category includes bartenders, janitors, homemakers and housemaids, and dishwashers. The presence of constant moisture damages the skin and makes it easy to tear or puncture it, allowing microbes easier entrance. In addition, moisture encourages the growth of fungi, leading to fungal infection of the nail and the nail bed.
Injury to the nail bed or the skin near the nails also breaks down the natural defenses offered by the skin and increases the likelihood of infection. This is especially so if the person is immunocompromised or diabetic. Thus biting or tearing off a hangnail is often associated with the development of paronychia because of the extension of the tear into healthy skin or into the nail bed, which predisposes one to infection.
Nail biting offers special conditions for infections of the nail folds because it not only produces trauma but also introduces bacteria from the mouth into the wound. This includes staphylococcus, streptococcus, pseudomonas and Gram-negative organisms, as well as fungi.
Eczema of the skin around the fingernails is also an invitation for secondary fungal or bacterial infection because of the broken skin and the moist conditions.
Constantly covering the nails is also bad for nail health. For instance, using sculptured (artificial) nails over your own nails cuts off the circulation of air from the area around them, encouraging infection. Similar is the case with prolonged use of plastic or vinyl gloves which trap moisture and restrict air entry around the nails.
How to do proximal nail fold infection Treatments Your Physician May Prescribe
For acute paronychia, your doctor may:
Puncture and drain the affected area and test for bacteria or viral infection.
Prescribe antibiotics for a bacterial infection or an antiviral medication for a herpes infection.
For chronic paronychia, your doctor may:
Prescribe a topical steroid.
Prescribe a topical antifungal medication.
Prescribe an oral antifungal medicine or antibiotics.
Related Items